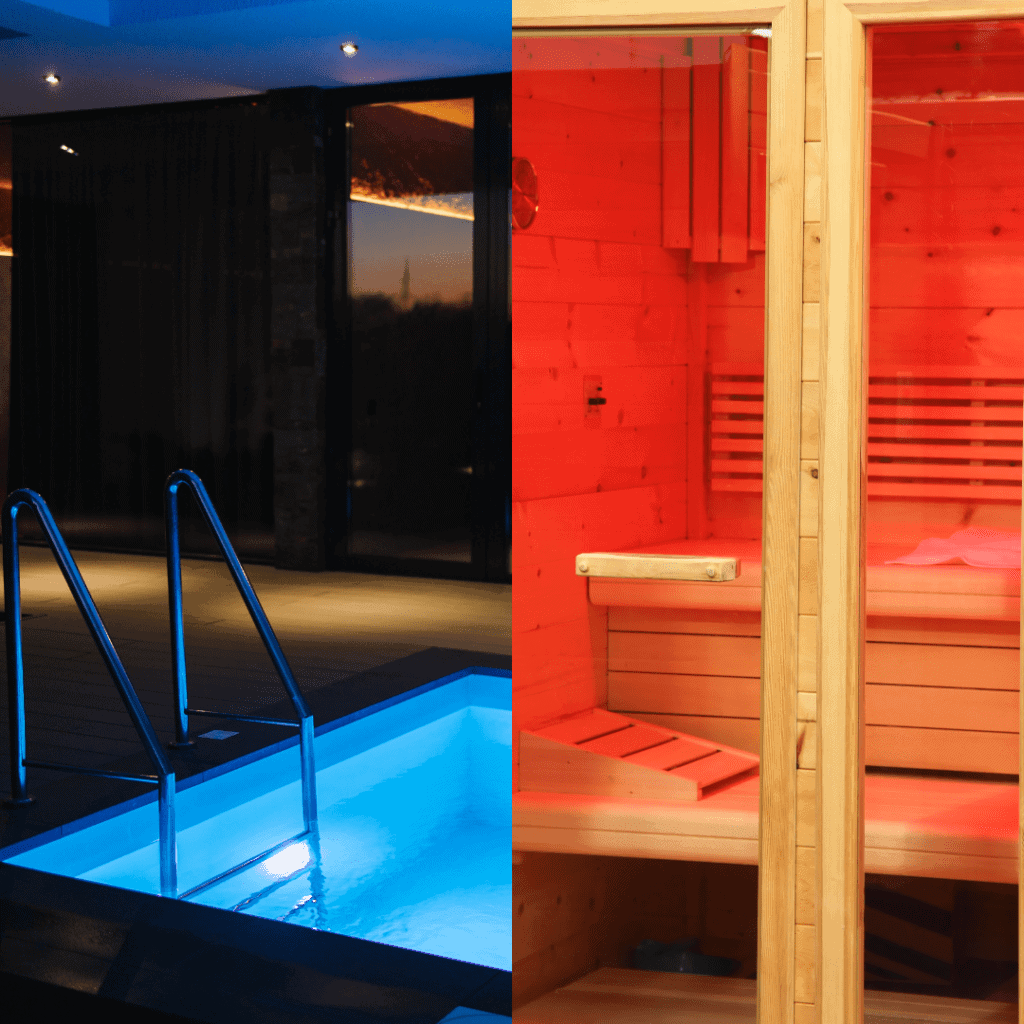
In the quest for optimal health and longevity, extreme temperatures have become an innovative way to tap into the potential of extreme temperatures. The contrasting practices of sauna bathing and cold exposure, often in the form of icy plunges, have gained significant attention due to their potential health benefits. These practices may seem like polar opposites, (pun intended) but they share a common thread in their ability to harness the power of temperature extremes to positively impact our bodies. In this blog, we will delve into the science behind the health benefits of sauna and cold exposure, while highlighting the role of Heat Shock Proteins (HSPs) in promoting longevity and musculoskeletal health.

The Heat is On: Sauna’s Therapeutic Powers
Saunas, originating from Finnish culture, involve sitting in a heated room often maintained at temperatures between 158 to 212°F (70-100°C). The experience induces profuse sweating, which has been linked to several health benefits. Notably, saunas stimulate the production of Heat Shock Proteins (HSPs), a group of proteins that play a crucial role in protecting cells from stress-induced damage. HSPs assist in protein folding, repair damaged proteins, and enhance cellular resilience.
A study published in the journal Frontiers in Pharmacology (2018) highlighted how regular sauna sessions can increase the expression of HSPs in cells, promoting cellular health and potentially extending lifespan1. Additionally, research from the University of Eastern Finland demonstrated that regular sauna use was associated with a reduced risk of cardiovascular diseases, sudden cardiac death, and overall mortality2.

Embracing the Chill: Cold Exposure’s Hidden Benefits
On the flip side of the temperature spectrum, cold exposure, often through cold water immersion or cryotherapy, has garnered attention for its potential health advantages. Cold exposure triggers a physiological response known as cold-induced thermogenesis, where the body generates heat to counteract the cold. This process stimulates energy expenditure and metabolic activity.
A study published in the journal Cell (2019) revealed that cold exposure leads to the activation of brown adipose tissue (BAT), a type of fat that generates heat to maintain body temperature3. This process is accompanied by the release of HSPs, which protect cells from cold-induced stress4.
The Longevity Connection: Heat Shock Proteins and Cellular Health
The common thread between sauna sessions and cold exposure is the role of Heat Shock Proteins in preserving cellular health. These proteins, which are induced by both heat and cold stress, serve as cellular chaperones, ensuring that proteins are folded correctly and cellular processes are optimized. This preservation of cellular integrity has significant implications for longevity.
Scientific Evidence: A study published in the journal Aging Cell (2017) explored the impact of HSPs on lifespan extension in worms and suggested that the induction of HSPs contributed to increased longevity5. This finding underscores the potential role of HSPs in promoting healthy aging across species.
Musculoskeletal Health: Finding Common Ground
While the primary mechanisms of action for saunas and cold exposure may differ, both practices converge on improving musculoskeletal health. Saunas, through the increase in blood flow and relaxation of muscles, can aid in reducing muscle soreness and improving flexibility. Cold exposure, on the other hand, can have analgesic effects, potentially reducing pain and inflammation.
Scientific Evidence: A study published in the European Journal of Applied Physiology (2014) examined the effects of cold water immersion on muscle recovery and found that it could effectively reduce muscle soreness and maintain muscle strength after intense exercise6. Additionally, a review in the Journal of Science and Medicine in Sport (2018) discussed how sauna bathing can improve joint mobility and reduce muscle tension7.
Not One Size Fits All
The debate of cold plunge versus sauna ultimately rests on individual preferences and goals. While saunas and cold exposure practices offer unique physiological responses, their common influence on Heat Shock Proteins and cellular health ties them together. Incorporating both practices into your wellness routine could potentially yield a comprehensive array of benefits, enhancing longevity, musculoskeletal health, and overall well-being.
As with any health regimen, it’s important to consult with a healthcare professional before embarking on new practices, especially those involving extreme temperatures. Embrace the fire and ice and consider experimenting with these contrasting yet innovative therapies. It’s best practice to gradually work your way into extreme temperatures as there are some dangers associated with excessive heat and cold like light headedness, dizziness, and dehydration.
Disclaimer: This blog provides general information and is not a substitute for professional medical advice. Always consult with a healthcare provider before making changes to your wellness routine.
Footnotes
- Leppäluoto, J., Tuominen, M., Vaananen, A., Karpakka, J., & Vuori, I. (2018). Increased Expression of Heat Shock Proteins in Human Skeletal Muscle After Training. Frontiers in Pharmacology, 9, 1473.
- Laukkanen, T., Khan, H., Zaccardi, F., & Laukkanen, J. A. (2018). Association Between Sauna Bathing and Fatal Cardiovascular and All-Cause Mortality Events. JAMA Internal Medicine, 178(6), 1-10.
- Chondronikola, M., Volpi, E., Borsheim, E., Porter, C., Annamalai, P., Enerback, S., … & Sidossis, L. S. (2014). Brown adipose tissue improves whole-body glucose homeostasis and insulin sensitivity in humans. Diabetes, 63(12), 4089-4099.
- King, N. A., Caudwell, P. P., Hopkins, M., Byrne, N. M., Colley, R., Hills, A. P., & Stubbs, R. J. (2007). Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. Obesity, 15(6), 1373-1383.
- Wang, M. C., Bohmann, D., & Jasper, H. (2003). JNK extends life span and limits growth by antagonizing cellular and organism-wide responses to insulin signaling. Cell, 121(1), 115-125.
- Leeder, J. D. C., van Someren, K. A., Gaze, D., Jewell, A., Deshmukh, N., Shah, I., … & Howatson, G. (2011). Recovery and adaptation from repeated intermittent sprint exercise. International Journal of Sports Physiology and Performance, 6(1), 27-41.
- Hannuksela, M. L., & Ellahham, S. (2001). Benefits and risks of sauna bathing. The American journal of medicine, 110(2), 118-126.