Magnetic Resonance Imaging (MRI) is a common type of imaging that allows practitioners to visualize more than the bones, setting it apart from x-rays as more detailed and informative. In fact, MRIs are so prevalent that since the first MRI in 1977, this type of imaging has climbed up to exceed 30 million studies performed annually (1).
How Does an MRI Work?
An MRI is performed through the use of magnetic fields and radio waves. These external forces interact with the fluids and tissues in the human body to create a series of recorded signals that create an image of the bones, tendons, ligaments, muscles, and tissues. Contrary to x-rays or Computerized Tomography (CT) scans, there is no radiation in an MRI. MRI is a popular form of imaging that can be performed more regularly to visualize changes in the studied tissues, without concern for excessive radiation exposure.
When Would I Get an MRI?
To summarize, MRI is a valuable form of diagnostic imaging because:
- It visualizes a variety of tissues, like bone, muscle, tendon and ligament
- It is a low-risk form of imaging, protecting the patient from accumulating exposure to radiation
- Repeat studies can be performed to assess changes to the area of interest
So, when would an MRI be warranted? In orthopedic medicine, an MRI would be performed when there is a medical necessity. Medical necessity varies depending on the nature of the injury. For example, if there is an acute, sudden, traumatic injury to the tissues in the body, an MRI would be warranted. However, if the issue has developed over time, there is a different pathway to discovering if an MRI is medically necessary.
The most important detail to note is “medical necessity” is ultimately determined by the insurance companies and the clinical pathways laid out by them as to when an MRI would be deemed a study the insurance company would pay for. Outside of insurance, a physician may determine an MRI is the best form of imaging to visualize the issue at hand.
Within the confines of medical necessity, a patient needs to exhaust conservative options, like physiotherapy and rest for six weeks. If the condition is still not significantly improved after six weeks of conservative care, the next step is an x-ray, and if the x-ray does not reveal any abnormalities, an MRI would be approved as a next step.
The steps between the patient’s onset of symptoms and insurance approval for an MRI is designed to eliminate unnecessary healthcare costs for avoidable imaging studies. If a patient responds positively to rehabilitation in a six-week period, the need for an MRI is eliminated because the patient’s pain and function has improved.
Also, what is even more noteworthy, is the high prevalence of significant clinical findings on an MRI in asymptomatic patients. This means that an MRI can reveal issues that are not even causing the patient pain or dysfunction. If a clinical finding appears in someone without symptoms, the image would drive or determine a need for a procedure or surgery that could be prevented. In fact, according to the 2020 article in Skeletal Radiology called Prevalence of abnormal findings in 230 Knees of Asymptomatic Adults using 3T MRI, “Nearly all knees (227/230; [97%]) of asymptomatic individuals showed abnormalities in at least one of the knee structures on MRI, of varying grades of severity” (3). Also, in shoulders, another study concluded:
Shoulder pathology is apparent in both symptomatic and asymptomatic shoulders and clinical symptoms may not match radiological findings. The cost burden of ordering MRI scans is significant and the relevance of the findings are questionable when investigating shoulder pain (4).
Another study found that in 98 subjects with no low back pain, 52% showed signs of asymptomatic degenerative disc disease on MRI (5).
The takeaway from this discussion on “when would I get an MRI?” is that an MRI should not be used as a conclusive diagnostic test determining the need for surgery or other interventional measures immediately. Many findings may be asymptomatic, not the actual pain generator, or correctable via conservative care, or less invasive routes than surgery.
3 MRI Findings that Matter in Regenerative Medicine
Now that we have determined that an MRI is a valuable test but not a ticket to needing surgery, there are several significant MRI findings we see routinely in our clinics Regenexx at New Regeneration Orthopedics of Florida offices.
These findings are significant, but not in the traditional sense of a finding that would suggest a need for surgery, for example. These findings are significant because they allow us to reverse engineer a cause to the painful problem at hand that can be corrected in addition to the regenerative procedure that would be most fitting for the patient.
1. Lumbar Spine: Multifidus Fat Atrophy
Back pain is a common complaint bringing patients into our offices in Tampa, Sarasota, St. Petersburg, and Orlando. Patients with back pain can present with either generalized low back pain, disc pain, or radicular pain. After we order an MRI, oftentimes the radiologist will comment on the health of the muscles stabilizing the lumbar spine.
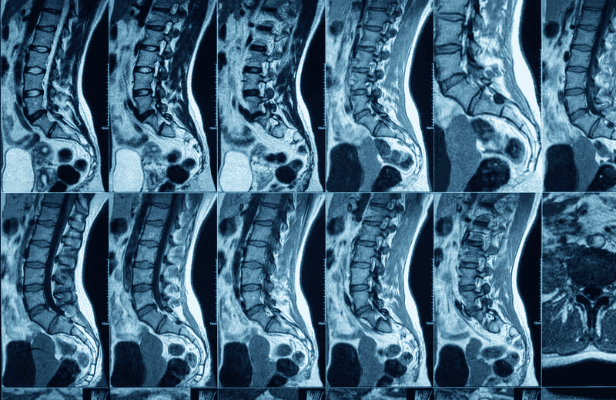
The back stabilizers include a large muscle called the multifidus that, when underutilized and weak, will become infiltrated with fat in a term called “fat atrophy.” This appears like marbling of fat within the muscles on MRI (Image 1). Fat atrophy is a telltale sign that the lumbar spine is not adequately supported by the surrounding muscles.
So, even though there maybe lumbar pathology that your regenerative physician will treat with Platelet Rich Plasma (PRP), there is also a need for the symptoms to be addressed with corrective exercise. To maximize the stability and support the PRP injections would do for the spine, the MRI-confirmed weak muscles need to be strengthened.
2. Knee: Chondral Defect and Bone Marrow Edema
A common occurrence with knee MRI is a patient complaint includes severe knee pain, limiting them from weight bearing activities they were recently doing, like running or walking. An example is a patient has sudden acute inflammation and swelling in the joint when walking, but there was no injury or known cause of this issue. In these cases, MRI typically does not show tears in the ligaments or tendons, but will report details like a “chondral defect” and/or “bone marrow edema”
A chondral defect means there is thinning or fissuring in the cartilage in the knee. Bone marrow edema is visualization of inflammation signals deep inside the bone of the knee (Image 2). A common term used to describe this finding is a “bone bruise,” but then the questions are: How did it form? and How do we correct it?
Bone marrow edema and chondral fissuring cases are usually fantastic candidates for regenerative medicine. Actually, pain generated from this type of knee pain has been studied over many years. Philip Hernigou performed 15-year comparison studies comparing the long-term effects of patients receiving a knee replacement versus interosseous knee injections and interosseous knee injections versus intra-articular knee injections. In both cases, there was a clinical significance in the outcomes of those receiving interosseous injections in both cases.
In traditional orthopedics bone marrow edema may be treated with just rest, or knee replacements may be suggested. However, our physicians would use a multifactorial approach of treating the issue with targeted interosseous injections as well as working with a physical therapist to correct the imbalances leading to these chronic injuries.
3. Tendon/Ligament: Partial-Thickness Tear
Tendons and ligaments are the structures of attachment in the body. Tendons connect muscles to bone and are responsible for force-generation from the muscle allowing us to move at our joints. Ligaments are the passive structures attaching bones to bones, creating stability in our joints. Bone structures are prone to damage in acute injuries, like an ankle sprain injuring the anterior talofibular ligament (ATFL) of the ankle or the anterior cruciate ligaments (ACL) of the knee. Tendons can be injuries in sudden injuries, or repetitive injuries.
If a tendon or ligament suffers a partial tear injury, it can cause pain, decrease function and be vulnerable to complete tearing over time. Additionally, the joint supported by the damaged tendon or ligament has less stability and then becomes more prone from repetitive stress arthritis.
Regenerative medicine procedures for partial ACL tears or partial rotator cuff tendon tears are effective options to replace surgery. The mechanism of these procedures is to specifically deposit PRP or bone marrow concentrate (BMAC), using ultrasound and fluroscopic-guided injections, to the void in the tendon to deposit the growth factors to help strengthen the damaged area.
The Takeaway?
MRIs are a form of imaging that reveal information of the status of myriad tissues in the joints that may be pain generators in your condition. Though an MRI may be a helpful diagnostic tool to help isolate the issue to treat, there are a lot of cases of “findings” on MRIs that may actually be asymptomatic. So, before jumping into a surgery after receiving an MRI result, it is important that the physician has also performed a physical and functional exam to identify the root cause of the issue.
At Regenexx at New Regeneration Orthopedics of Florida, our physicians pair MRI findings with a physical exam, functional exam, a detailed history, an ultrasound exam, and an hour-long new patient evaluation. Then, the nuanced MRI findings like fat atrophy, bone marrow edema, or partial tendon tears can be addressed with a multifaceted approach of evidence-based regenerative procedures and targeted functional rehabilitation.
If you have questions about what your MRI result means for your injury, or are interested in avoiding an unnecessary surgery, a new patient evaluation with one of our physicians would be a great place to start.
References:
- https://www.envrad.com/facts-about-mris/
- https://www.radiology.ca/article/when-mri-appropriate/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7237395/#:~:text=Nearly%20all%20knees%20(227%2F230,of%20varying%20grades%20of%20severity.
- https://onlinelibrary.wiley.com/doi/full/10.1111/1756-185x.12476
- https://ard.bmj.com/content/62/4/371
- https://regenexx.com/blog/is-there-solid-research-on-using-prp-to-treat-spinal-pain/
- https://newregenortho.com/15-year-studies-suggest-new-regenerative-medicine-standards-for-advanced-knee-arthritis/
- https://regenexx.com/conditions-treated/knee/acl/#:~:text=Both%20partial%20thickness%20and%20full,surgical%20repair%20to%20heal%20properly.
- https://regenexx.com/conditions-treated/shoulder/rotator-cuff-tear/